More than 99% effective – one of the most effective forms of contraception. A Fit & Forget Contraception. There are two funded hormonal IUDs in New Zealand – Mirena and Jaydess.
There are two main types of IUDs – hormonal and non-hormonal. This page provides information on the hormonal IUD. For information on non-hormonal IUDs, click here.
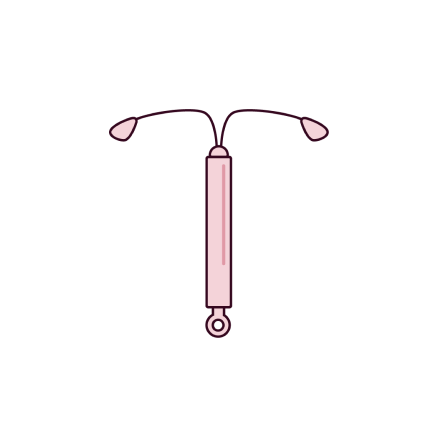
The hormonal IUD is a small, T-shaped plastic device which contains the hormone progestogen. It slowly releases this hormone into the uterus.
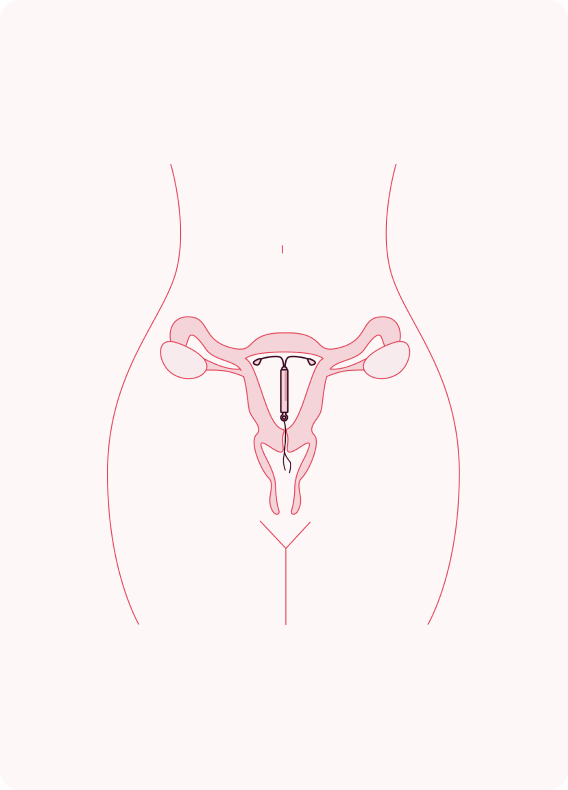
It is placed in the uterus.
There are two funded hormonal IUDs in New Zealand, Mirena and Jaydess.
The hormonal IUD uses a hormone called levonorgestrel. It slowly releases this hormone into the uterus.
It prevents pregnancy by preventing the egg being fertilised by sperm, by:
A trained nurse, midwife, or doctor fits the IUD in your uterus.
The image shows the position of the IUD in the uterus. The strings from the IUD will not be visible.
There are loads of things about Hormonal IUDs that are good for your body as well as your sex life.
Lots worry about negative side effects, but for many people, they’re not a problem. Most people adjust to having a hormonal IUD pretty quickly but give yourself time. It could take a few months.
A hormonal IUD needs to be fitted by a nurse, midwife or doctor who has been specially trained. It is available FREE* from a range of services.
Most people can use an IUD, including those who are young and those who have not been pregnant before. Your nurse, midwife or doctor will advise you of the best option for you to choose.
An appointment will typically include:
Fitting the IUD (shouldn’t take longer than 5 minutes):
You are likely to get some period-type pain and possibly some light bleeding for a few days afterwards.
The IUD has two threads which hang through the opening at the entrance of your uterus (cervix). You could check the threads a few times during the first month and then at least once a month.
Once the IUD is fitted, you may need to go back to the doctor, midwife or nurse after three to six weeks for a check up.
It is very unlikely that the IUD will come out but if you are worried and can feel the IUD itself, or cannot feel the threads you should see a nurse or doctor straight away.
You will then only need to go back when the IUD needs to be replaced (3 to 5 years depending on the type).
You should go back to the nurse, midwife or doctor if you notice any of the below symptoms:
The hormonal IUD can be fitted at any time in your cycle if it is certain that you are not pregnant.
As soon as the hormonal IUD is fitted then you will be protected immediately. You will be asked to take a pregnancy test before the IUD is fitted and another three weeks later if there is a pregnancy risk.
The hormonal IUD must be removed by a trained nurse, midwife or doctor, the procedure
should be less painful and quicker than having the IUD fitted. Your nurse or doctor can take out
your IUD by putting a speculum into your vagina and gently pulling on the IUD strings.
If you are not going to have another IUD you will need to use additional contraception, such as
condoms, for the seven days before the IUD is taken out if you do not want to become
pregnant.
Your fertility should return to normal as soon as the hormonal IUD is removed.
While using the IUD you can use tampons and/or sanitary pads.
No neither you or your partner should feel your IUD. An IUD is positioned in the uterus. You may be able to feel the strings in your vagina and your partner may notice the strings during sex. The strings of the IUD usually get softer over time, but if they’re really a problem, talk to your doctor, midwife or nurse about adjusting them or cutting them shorter.

Note: Wāhine/women+ includes consideration of whānau and social context and is intended to be inclusive of gender diverse people who share some of the health needs of women but do not identify as women. (RANZCOG, 2022)
The development of this website was supported with an educational grant from Bayer.
Copyright © Protected&Proud. All Rights Reserved.
A non-hormonal (Copper) IUD is a small, T-shaped plastic device which contains copper. It is put into the uterus (womb). A Copper IUD does not contain hormones. The copper IUD can also be used as an Emergency Contraception.
LASTS FROM 5 TO 10 YEARS | PLACED IN THE UTERUS | EFFECTIVE IMMEDIATELY | EMERGENCY CONTRACEPTION – UP TO 5 DAYS AFTER SEX
A Hormonal IUD is a small, T-shaped plastic device, which contains the hormone progestogen to control your fertility. The device is put into the uterus (womb).
HORMONES | LASTS FROM 3 TO 5 YEARS | PLACED IN THE UTERUS | EFFECTIVE IN 7 DAYS
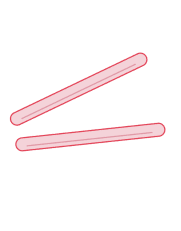
Two small, flexible plastic rods that are placed just under the skin in the upper arm. The implant releases the hormone progestogen to control fertility.
HORMONES | LASTS UP TO 5 YEARS | PLACED IN THE ARM | EFFECTIVE IN 7 DAYS