There are two types of condoms – male and female (internal) condoms. Condoms protect against unwanted pregnancy and STIs. Condoms are also known as barrier methods.
There are two types of condoms – the male condom and the female (internal) condom.
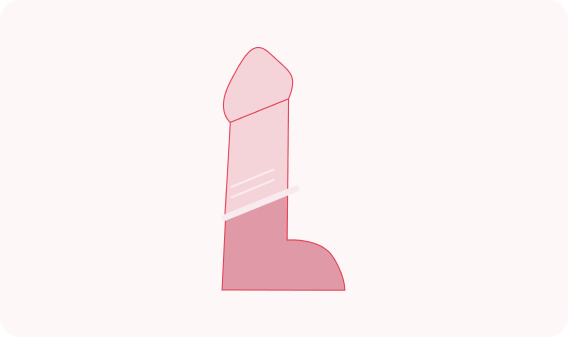
Male condoms protect against unwanted pregnancy by stopping the sperm contained in semen coming into contact with the vagina (which could lead to an egg being fertilised).
A male condom covers the penis and acts as a barrier between it and the mouth, vagina, penis or anus. This prevents sexual fluids being transferred between partners, which provides protection against sexually transmitted infections (STIs).
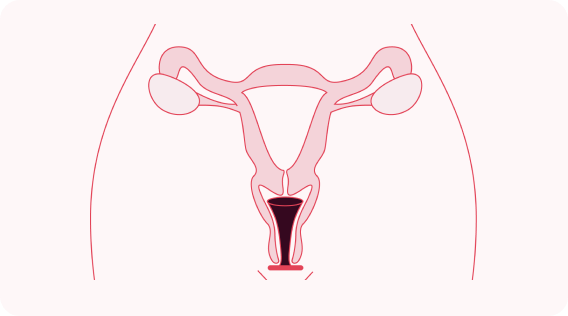
Female condoms line the vagina and protect against unwanted pregnancy by stopping the sperm contained in semen coming into contact with a vagina (which could lead to an egg being fertilised).
They also stop sexual fluids being transferred between partners which provides protection against STIs.
Condoms are available from healthcare professionals as well as to buy from retail/online shops. You can get a prescription for condoms from your nurse or doctor. Prices vary depending on where you go and the appointment fee in place. Click here to find your nearest service.
If the condom has broken, split, slipped off or you’re worried it was used incorrectly, you should get checked for an STI test and emergency contraception if there is a risk of unwanted pregnancy.

Note: Wāhine/women+ includes consideration of whānau and social context and is intended to be inclusive of gender diverse people who share some of the health needs of women but do not identify as women. (RANZCOG, 2022)
The development of this website was supported with an educational grant from Bayer.
Copyright © Protected&Proud. All Rights Reserved.
A non-hormonal (Copper) IUD is a small, T-shaped plastic device which contains copper. It is put into the uterus (womb). A Copper IUD does not contain hormones. The copper IUD can also be used as an Emergency Contraception.
LASTS FROM 5 TO 10 YEARS | PLACED IN THE UTERUS | EFFECTIVE IMMEDIATELY | EMERGENCY CONTRACEPTION – UP TO 5 DAYS AFTER SEX
A Hormonal IUD is a small, T-shaped plastic device, which contains the hormone progestogen to control your fertility. The device is put into the uterus (womb).
HORMONES | LASTS FROM 3 TO 5 YEARS | PLACED IN THE UTERUS | EFFECTIVE IN 7 DAYS
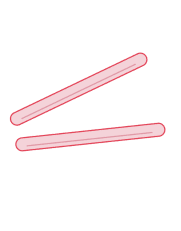
Two small, flexible plastic rods that are placed just under the skin in the upper arm. The implant releases the hormone progestogen to control fertility.
HORMONES | LASTS UP TO 5 YEARS | PLACED IN THE ARM | EFFECTIVE IN 7 DAYS